We interviewed Dr. Colleen Reichmann to find out more about what it’s like to be a therapist who specializes in eating disorders.
Q: Why did you become a therapist?
I became a therapist because, quite simply, I wanted to give back! I have struggled with my own mental health issues, and have seen first hand the healing power of therapy, which inspired me to pursue a career in psychology.
Q: What made you decide to go into eating disorder treatment as your specialty?
I mainly made this decision because of my own past history-I struggled with an eating disorder for around a decade. I was told that I would be a “chronic” patient and felt so hopeless at times. When I finally began to really recover, I realized that I wanted to use this journey to help others who are struggling with eating disorders. This is not to say that I understand your eating disorder, because everyone is different. My past history simple gives me what I like to call an “empathy chip” for this particular illness and journey.
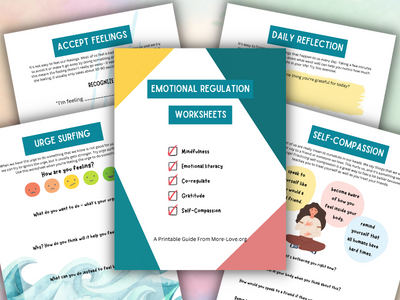
Emotional Regulation Worksheets
Give these printable worksheets to grow more confident, calm and resilient and feel better, fast!
- Self-Esteem
- Self-Regulation
- Mindfulness
- Calming strategies
Q: What training have you received to be an eating disorder specialist?
Unfortunately, I did not receive much specialized training in the core parts of my graduate program, as it was a generalist program. I sought out research experiences (assistantships and my masters thesis and dissertation) that focused on eating disorders. I also attended conferences and trainings outside of school as much as I could. I completed my predoctoral and postdoctoral internships at inpatient eating disorders units, which were huge training experiences. Currently, I am pursuing my CEDS specialist, and expect to be finished within a year or so!
Q: How do you pursue ongoing education as an eating disorder specialist?
I attend conferences. Specialized eating disorder conferences are absolutely crucial. I make it a point to find training opportunities that offer an inclusive, Health At Every Size perspective on issues within the ED community.
Q: How do you typically approach treating a child (up to age 18) for an eating disorder?
Typically I utilize family based therapy (FBT) if at all possible. (I have received some specialized training in FBT). If parents are invested, involved, and ready to learn, I find it is ALWAYS best to include them in the treatment process. After all, you know your child far better than I do! If this is not possible, I offer interpersonal/feminist-relational therapy, with cognitive behavioral therapy techniques threaded throughout. I believe that insight-focused work AND behavior/action-focused work is necessary when it comes to recovery from an eating disorder.
Q: What treatment format do you typically recommend for a child (up to age 18)? For example, how often do you like to meet, for how long, and do you involve family members? Do you involve other caregivers like doctors and nutritionists?
I recommend at least weekly individual session, (50 minutes each), and every other session would ideally involve parents. I also recommend monthly (or more if needed) meetings with an eating disorder-informed MD, and weekly meeting with a dietitian (pediatric dietitians are very helpful for children under 12/13), and non-diet, fat-positive dietitians for everyone else!
Q: What would you like parents to know about having a child who has an eating disorder?
I would like parents to know that this is not your fault. This is a serious mental illness with research-proven genetic underpinning. You cannot “give” your child an eating disorder. You can, however, be a powerful piece of their recovery. I would also like to remind parents who feel helpless/powerless that you likely fed your child successfully for many years. You have the power and the knowledge to help your child-all you need now is guidance and support in how to apply that power now that your child is struggling with an ED.
Q: What mistake(s) do you think parents make when parenting a child who has an eating disorder?
I commonly see parents trying to “appease” their child when it comes to recovery. This is understandable-if your child is begging you not to eat something, to make something different, or to eat less, it is so common and human to want to comfort your child by giving in. To this I say, much like other aspects of parenting, the most comforting action for your child is not what will be best for him/her/them in the long term. Empathic firmness works best here.
I also see parents trying very hard to understand the eating disorder or rationalize what is happening to their child. Often times, it is impossible to find the rationality in someone who is struggling with an eating disorder. Please know that this is an illness with a largely fear-based brain component. Meaning that, neurochemically, your child’s brain is likely reacting similarly around food to someone who struggles with an extreme phobia and is being asked to confront it. So please do not feel hopeless if explaining the rational need for food/eating does not get through to your child.
Q: Do you see any promising new research or techniques that you think will make an impact on the future treatment of eating disorders?
I have recently seen some research that involves “bridging the gap” between research and field work when it comes to family based therapy. (This “gap” refers to the difference between the great outcomes that we have seen in controlled studies, versus the less-powerful outcomes that we see when this research is applied to real-life clients). I think this idea of focusing on the gap and how to close it will be very helpful to the field.
Additionally, we are seeing more and more providers discussing the role of intersectionality, identity, oppression, and marginalization when it comes to eating disorders. This is helpful because it allows us to begin addressing and confronting the environment that leaves some people vulnerable to eating disorders. (Versus acting as if recovery happens in a vacuum).

Colleen Reichmann, Psy.D. is a licensed clinical psychologist who specializes in the treatment of individuals with eating disorders and body image issues. She has worked at various inpatient eating disorder treatment facilities and is the blog manager for Project HEAL. She lives in Virginia Beach with her husband and golden doodle and currently works at a group practice.